The modern healthcare has seen a transition from disease-centered to patient-centered care, and this change is part of the National Quality Agenda in the United States. Also called family- or user-centered, individualized or personalized care, it means putting patients and their relatives at the heart of medical decision-making and regarding them as experts who should work together with clinicians to reach value-based outcomes.
The major aspects of such care include patient engagement and education, accessibility and personalization of care, and regular, effective communication.
At the policy level, enhancing patient experience has become a component of the Triple Aim (“Better Health, Better Care, Lower Cost”) of the US healthcare, and the patient-centered care has been already implemented across many programs as mandated in the Patient Protection and Affordable Care Act (ACA). These are the programs initiated by the Centers for Medicare and Medicaid Services (CMS), the Society of Critical Care Medicine (SCCM), the Patient-Centered Outcomes Research Institute (PCORI), and other organizations.
With the abundance of technologies offered by the global healthcare IT market and the adoption of relevant policies and regulations, sustaining patient-centered care becomes easier.
EHRs to foster accessible care
The Centers for Medicare and Medicaid Services have a long, rich history. Their programs have been providing health coverage to vulnerable US population — the older, disabled, and low-income people — since 1965. Yet, it’s been relatively recently that the organizations woke up to the necessity to underpin their programs with technology.
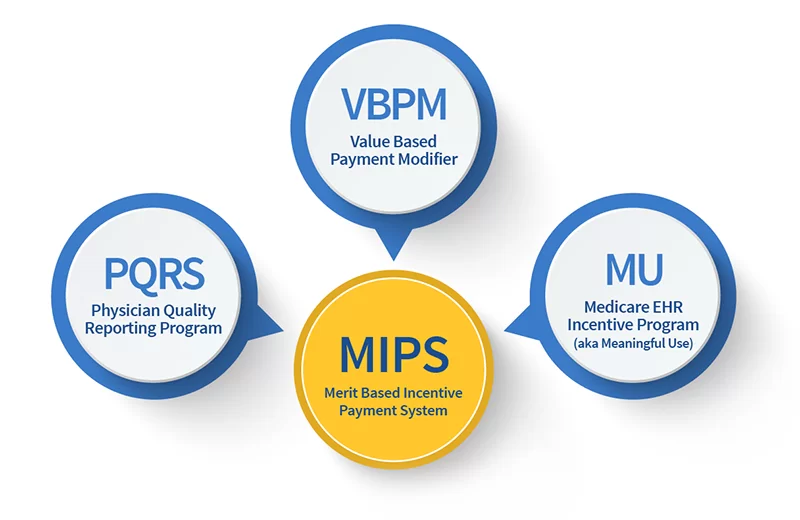
In 2011, the CMS spearheaded the EHR Incentive Programs to encourage eligible professionals, eligible hospitals, and critical access hospitals to adopt, implement, and demonstrate the meaningful use of certified EHR technology.
The current 96% EHR adoption rate is clear proof that the programs caught on quickly. While increasing their financial efficiency, EHR-enabled healthcare organizations managed to improve population health by serving more patients and shortening their hospital stay.
The next step that can immensely contribute to care accessibility is to include social determinants of health (SDOH) and behavioral indices in EHRs. These are not only alcohol and tobacco use, race, and residential address, but also education, physical activity, stress and depression, social isolation, income, domestic violence, and other aspects.
This undertaking is set to optimize Medicare and Medicaid payment models, at the same time accelerating decision-making, facilitating coordination with community-based organizations, enabling faster referrals, and reducing health inequalities.
Empowering patients through information
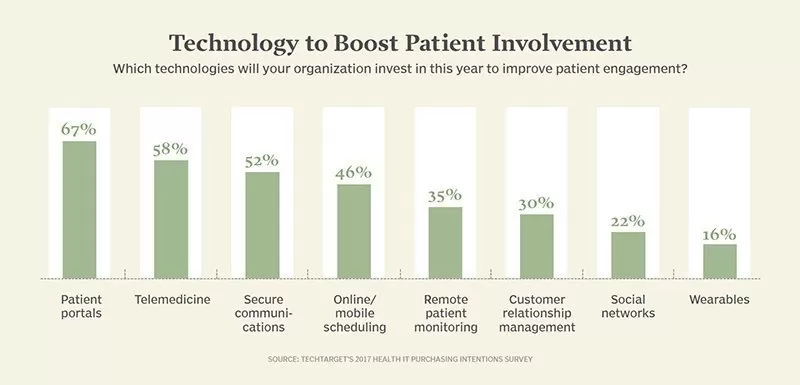
As the Healthcare Information and Management Systems Society (HIMSS) puts it, “a patient’s greater engagement in healthcare contributes to improved health outcomes, and information technologies can support engagement.” Here’s an overview of solutions developed so far toward that end.
Medical portals
One of the possible EHR extensions, a medical portal is considered the most popular method of patient involvement — according to a survey done by the New England Journal of Medicine. This solution empowers patients to access a range of useful functions, including appointment scheduling, e-consultations and chats with physicians, requests for prescription refills, as well as checking for medications, test results, and allergy lists.
However, to bring tangible value, a patient portal needs to be accessible for people of all abilities and on any device, allow for seamless integration with third-party systems, provide multimedia educational resources, enable notifications, and facilitate invoice management.
Athenahealth, a US-based health IT vendor, admits that the increased portal adoption rate in its healthcare network has positively impacted business results, including a higher average patient pay yield.
Personal health records
Patient health records (PHR) go a step further than medical portals. While a portal is fully controlled by an EHR administrator, a PHR system is at a patient’s and their family’s disposal and isn’t necessarily connected to a hospital.
With such a solution in place, patients can individually combine and coordinate protected health information (PHI) from multiple health providers — thus building a full picture of their medical history and overcoming software interoperability barriers.
Additionally, the wider PHR adoption is, the more patients can increase their awareness of radiation exposure risks arising during imaging procedures. To wit, seven vendors found success with the RSNA Image Share Program, which lets clinicians share radiology reports via a patient’s PHR account.
Patient-generated health data
With IoT healthcare solutions on an upswing, an efficient use of patient-generated health data (PGHD) in hospitals doesn’t seem far-fetched.
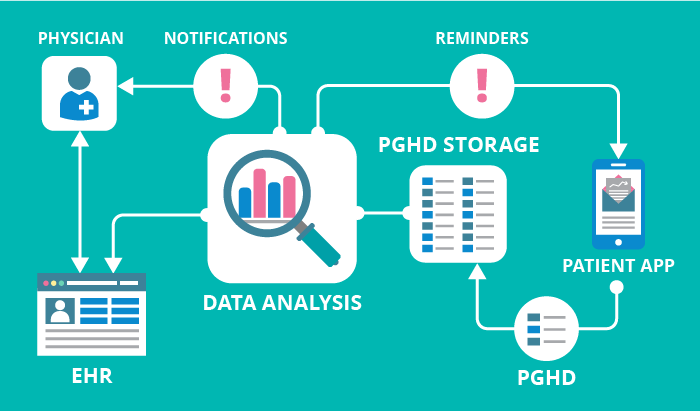
Once this data — for instance, blood pressure, weight, or glucose levels — is successfully incorporated into healthcare software systems, physicians will be able not only to empower and engage patients but reap other benefits. These include refining chronic disease management, optimizing treatment plans, speeding up decision-making, and balancing operational costs.
Other things that need attention
With EHR systems, medical portals, PHRs, and PGHD, technology is significantly contributing to patient-centered care. Still, there are some things to keep in mind when adopting these solutions, mainly security and interoperability.
First, any system that contains PHI and/or is used by covered entities and their business partners should be developed in strict compliance with the HIPAA Security and Privacy Rules. Second, as data exchange still needs work, particular attention should be paid to the FHIR standard and open APIs.
Healthcare software vendors stay in the loop regarding these security and interoperability standards, which helps them provide clinicians with workable solutions.
Summing it up
Technology is helping to redefine the patient’s role in care delivery, yet with it come more benefits both for patients and their healthcare providers, such as broader care accessibility, increased personalization, improved communication, and reduced health disparities.
And once the interoperability and security challenges are addressed, health institutions will find it much easier to focus on how informed and engaged their patients are — to keep patient-centered care on the agenda.